In the 1970s, Japanese automakers overtook their U.S. counterparts largely due to a focus on quality. Taking human interaction out of numerous processes enhanced the reliability of the automobile and catapulted them into a dominant share of the market. Unfortunately, healthcare organizations don’t have that same luxury. As hospitals and patient care organizations tackle quality and patient safety, the human element remains an essential part of the process.
Quality And Patient Safety Costs
Although quality and patient safety remain the priority for healthcare organizations, eliminating errors isn’t easy. Current estimates place the patient safety death toll at approximately 250,000 people annually in the United States, with a total patient harm cost of more than $17 billion. (Makary & Daniel, 2016; Van Den Bos et al., 2011). And turnover adds to this challenge. According to the National Healthcare Retention & RN Staffing Report, the average hospital turnover rate in 2019 was 17.8%.
Quality And Patient Safety Improvements
In healthcare, quality improvement is a part of everyone’s workday. Although technology advancements and new processes may generate a jump in performance, by nature, these advancements are few and far between. But as important as breakthrough processes are, incremental improvements, which can occur routinely, will have a profound impact over the long term. As James Cleary details in his book, Atomic Habits, there is a surprisingly narrow gap that separates the good performance from the great performance. And that narrow gap is separated by small habits and daily rituals. Developing daily rituals, focusing in areas with ongoing patient safety challenges, or adding these following elements to your routine, will impact the quality of care you deliver.
Medication Safety
Prescription drugs and other medications are important for many adults. In fact, the majority of adults take a prescription medication today. Communicating medication safety is important, challenging and one that requires constant attention.
Drug Shortages
The FDA currently lists shortages for over 100 different drugs. And with supply chain issues, especially those experienced during COVID-19 disruptions, establishing processes to prepare for, communicate and monitor these situations are crucial to avoid adverse drug events.
Drugs WIth Unusual Dosage
In the last 30 days nearly half of U.S. adults took a prescription drug. And the dosage for most of these fall into the “normal” category. But, some have unusual dosage requirements. For example, Methotrexate, a drug originally approved for cancer treatment is now used to treat autoimmune diseases like severe rheumatoid arthritis. But, the treatment regimen is unusual, only one dose per week. As a result, inadvertent daily dosing occurs, with some frequency, both at the point of prescription and with self-administration. Methotrexate overdoses can have serious repercussions ranging from vomiting to life-threatening pulmonary symptoms.
Medication Instruction
But, the problem goes beyond drugs with unusual dosage requirements. Recent data from the Centers for Disease Control and Prevention, published in the Journal of the American Medical Association, indicates that four visits to the ER per 1,000 adults annually are due to adverse drug effects. With almost 60% of Americans taking at least one prescription drug and nearly 20% taking more than five, the challenge is far reaching. Minimizing medication errors takes various forms of communication directed at both the provider and the patient.
Peripheral intravenous Catheters (PIVCs)
Peripheral intravenous catheters (PIVCs) are the most widely used invasive devices among inpatients. In fact, healthcare providers use an estimated 200 million peripheral intravenous catheters in the US each year, making them the most common form of IV treatment.1 Although PICC line utilization is increasing, they are not without risks and potential complications.
Medication Safety Daily Rituals
These steps can help you address the ongoing medication safety challenges that both healthcare professionals and patients experience on a daily basis:
1) Drug Shortages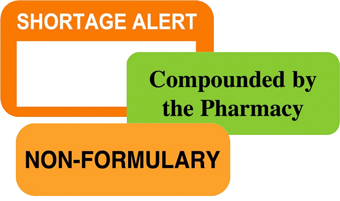
Minimizing the impact of drug shortages starts with monitoring medications. Identifying those in short supply, assessing purchase history, estimating usage and pinpointing alternatives will allow you to better manage supply chain issues. In addition, it’s important to routinely inventory medications to ensure visibility into medications that are available and those that are not.
2) Medication Instructions And Unusual Drug Dosage
Regardless of whether the medication has a common or unusual dosage, verify prescription dosage strength when updating a patient’s medication history and when refilling prescriptions. In addition, provide patients oral and written instructions that specify the dosing schedule and mark prescriptions with specific instructions.
3) Peripheral Intravenous Catheters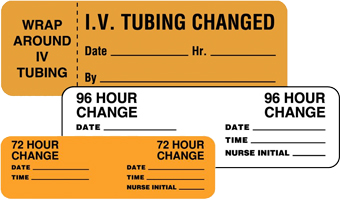
In addition to inserting the central line properly, healthcare providers must use stringent infection control practices each time they check the line or change the dressing including:
- Perform hand hygiene
- Apply appropriate skin antiseptic
- Ensure that the skin prep agent has completely dried before inserting the central line
- Use five sterile barrier precautions:
- Sterile gloves
- Sterile gown
- Cap
- Mask
- Large sterile drape
Infection Prevention And Control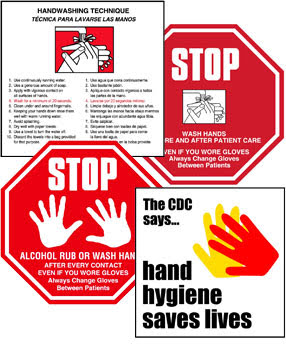
As healthcare organizations strive to achieve high reliability in all care areas, there is one that consistently falls short - hand hygiene. In fact, with most quality and patient safety processes across healthcare organizations ranking in the high 90 percentiles, hand hygiene hovers around 60. In addition to these challenges, because of COVID-19, aerosol-generating procedures came into greater scrutiny. Although healthcare workers were more vigilant and adhered to infection prevention processes in 2020, mitigation remains an ongoing challenge.
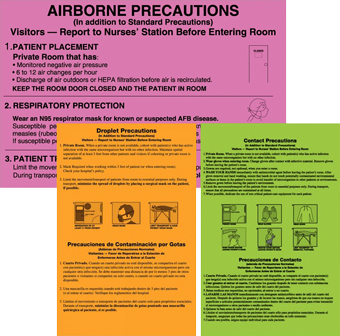
Infection Control For Aerosol-Generating Procedures
Managing these risks starts with minimizing the transmission risk factors during procedures and reducing the length of exposure and proximity to the patient’s airway and/or the aerosol.
 Personal Protective Equipment
Personal Protective Equipment
Personal protective equipment (PPE) is clinically proven to reduce the spread of infection and its importance accelerated as COVID-19 overtook the healthcare system. But, it doesn’t diminish the need to prioritize its use in all applicable areas. It remains an essential step in decreasing bacteria colony forming units (CFUs).
 Catheters, Dialysis Machines And Medical Devices
Catheters, Dialysis Machines And Medical Devices
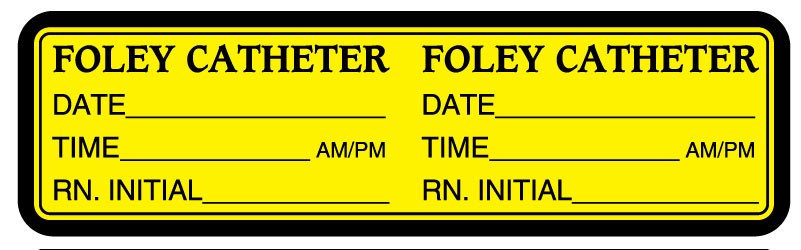
Urinary tract infections are now the most common type of HAI and approximately 75% of these infections are associated with the insertion of a urinary catheter. Plus, dialysis machines are another infection hot spot.
Infection Control Daily Rituals
Infection prevention requires procedures and policies aimed at the root cause. Direct contact with bacteria and other types of germs, usually by the hands, is the most frequent mode of infection transmission.
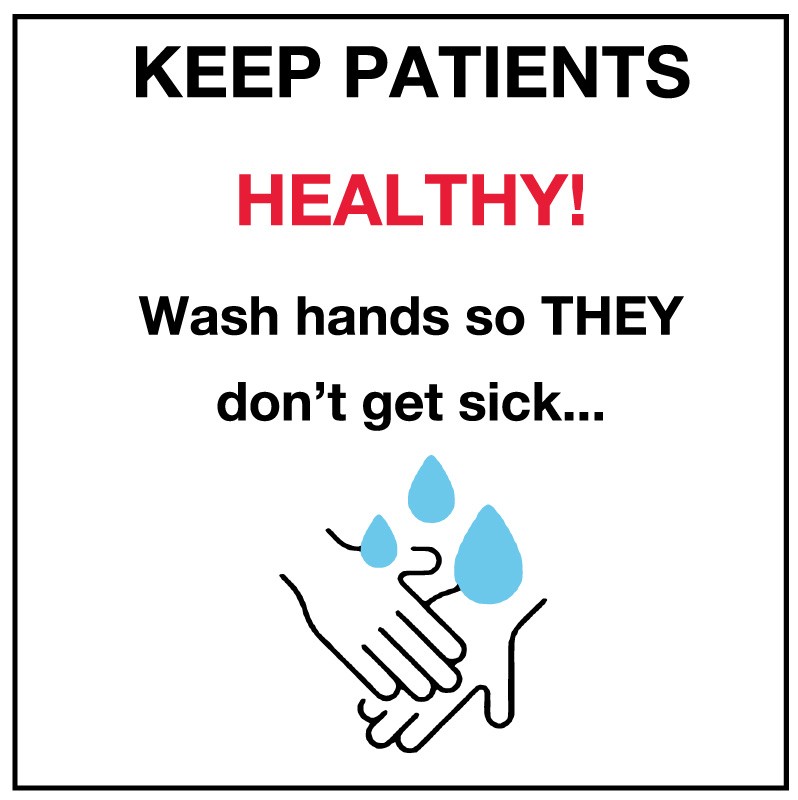 1) Hand Hygiene
1) Hand Hygiene
Hand hygiene, or lack of, remains the primary culprit of infection control. But, setting expectations and using ongoing reminders that encourage patients, visitors and staff to wash hands have proven effective. Plus, messaging that focuses on preventing patients from catching viruses motivated healthcare professionals to wash their hands at a higher frequency than other messages. Place reminders in high traffic areas and in bathrooms and other spots where germs are more likely to populate.
2) Aerosol Generating Procedures
Minimizing aerosol generating procedures starts with implementing controls. Steps including:
- Using negative-pressure air systems
- Schedule aerosol-generating procedures for the end of the day
- Test patients for COVID-19 before their procedures
- Restrict personnel and visitors in the room, and train staff on risk reduction and personal protective equipment (PPE) Have proven to decrease potential virus transmissions.
3) Personal Protective Equipment
Personal protective equipment effectiveness is similar to hand hygiene in this sense, it only works when you use it. Ensure the use of eye protection, gowns, gloves, masks, and respirators when administering aerosol-generating procedures. In addition, use visual reminders of pending hazards to communicate appropriate precautions.
Catheters, Dialysis Machines And Medical Devices
Like many infection control processes, regular cleaning and disinfecting reduces infection risk. This is true for the equipment and the surrounding environmental surfaces. Dirty/clean tapes are a good way to show the equipment status. Also, changing catheters on a regular schedule reduces infection risks. Using catheter change reminders inform staff of the proper changing times. In addition, dialysis machines are another infection hot spot. A checklist like this helps serve as a guide ensuring the medical staff takes the proper cleaning, disinfecting and hand hygiene steps.
Improvised Use Of Medical Device
Although healthcare providers may need to modify how they use a medical device, changing from the standard can lead to serious safety and regulatory compliance issues. Repurposing a medical device, workflow, or system starts with documenting equipment limitations, failures, user errors, and improvisations that may affect patient care.
 Medical Device Daily Rituals
Medical Device Daily Rituals
Implement preventive maintenance programs that include regular quality and patient safety assurance checks to monitor device safety. After making those checks, communicate the equipment status by adding the important safety, maintenance, calibration and inspection information for staff to see.
Emergency Preparedness
As our reliance on digital processes continues to increase, it elevates the challenges healthcare organizations face when system outages occur. Both cyber attacks and natural disasters are increasing in frequency. It pays to prepare for what is likely an inevitable outcome.
Cyber Attacks
Already 2021 has seen a dramatic increase in cyberattacks. System outages experienced at Scripps and CompuGroup Medical are just two of the recent high-profile attacks against healthcare organizations which continues a trend from 2020. In fact, Health IT Security reported that 560 healthcare organizations were hit with cyber attacks in 2020. Even in high tech organizations, it’s often something obvious like a weak password that allows cyber criminals to break into a company's IT infrastructure. As a result, organizations are implementing a zero trust security concept.
Natural Disasters
Equally as unpredictable as cyber attacks are natural disasters. But just like cyber attacks, they are increasing in frequency. The U.S. government’s national climate assessment found weather extremes are on the upswing. Heavy precipitation events that cause flooding, Atlantic hurricane activity and wildfires in the Western United States are escalating. Evacuation planning, identifying alternate care sites, assisting vulnerable populations such as dialysis and home ventilator patients are just a few of the adjustments to consider. So as extreme conditions become the norm, the importance of hospital emergency management planning increases along with it. And although natural disasters have a broader impact on healthcare facilities, the Joint Commission "all hazards" approach is one way to prepare for emergency management. This allows you to prepare for a range of emergencies varying in scale, duration, and cause.
Emergency Preparedness Daily Rituals
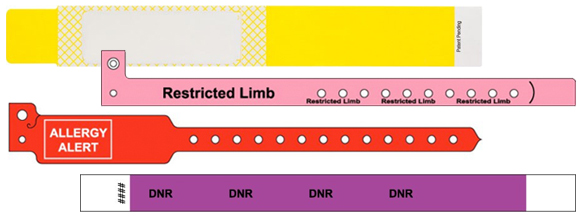
Throughout the entire spectrum of patient care, digital processes drive the workflow. But, with EHR systems unavailable or with lost or limited power, switching to manual processes may be the only option. So evaluate access to supplies on a routine basis. Maintaining an inventory of items including
- Manual admission documents and patient wristbands
- Patient care communication labels
- Pharmacy labels
- Lab test labels
- Discharge checklists
- And more Allow you to communicate essential information to the clinical staff when patients require ongoing care.
Improving Patient Safety In Hospitals
It is easy to dismiss the value of making slightly better decisions on a daily basis. Sticking with the fundamentals or getting one percent better doesn’t make the headlines. But despite its lack of allure, the most important part is taking this approach works.
United Ad Label
Although leadership paves the way to improved patient safety in hospitals, and throughout all healthcare organizations, improvements are part of everyone’s workday. United Ad Label plays a small but important role in that improvement process. Our products guide proper medication dispensing for both the clinical staff and patients, encourage staff, patients and visitors to take proper precautions to minimize the spread of infections, help you operate when systems are down and more.