Care delivery is a complex process and one that compounds in complexity when variables are introduced. In fact, facilitating safe and effective care depends upon two key factors: the knowledge and skills of the clinical staff and care delivery design. That’s why healthcare organizations employ process standardization. Because as the uniformity of essential clinical care functions increases, the potential for errors decreases. That’s why care delivery design enhancements from information technology workflows to standardizing medication labels can improve patient care.
Standardizing Key Processes Reduces Patient Errors
In addition to the complexities, modern healthcare is also high risk and error-prone. What’s more, the World Health Organization (WHO) reports that:
- 4 out of 10 are harmed in primary and ambulatory settings
- 134 million adverse events occur each year
And not surprisingly, errors and consequent adverse events are a leading cause of death and injury.
Furthermore, ongoing changes in the healthcare landscape create a different set of challenges. For example, as health systems grow or merge, and the number of clinical staff that serve various facilities multiply, the potential to inject variables into care delivery increases.
But, standardizing key processes has proven to reduce these problems. In fact, Idaho based St. Luke’s Health System found that reducing care variations helped them achieve:
- 13.4% fewer in-hospital deaths
- 8.5% fewer complications
- 10.2% shorter lengths of stay
Medication Errors And Adverse Drug Events (ADEs)
The Agency For Healthcare Research And Quality reports that nearly 5% of hospitalized patients experience an ADE, making them one of the most common types of inpatient errors. Further, ambulatory patients may experience ADEs at even higher rates.
Reducing medication errors requires ongoing vigilance and standardizing medication labels is one part of that process. But for standardization to succeed, it must incorporate formats and procedures that work effectively with EHRs.
Standardizing Medication Labels
From oral delivery to injections and ongoing IV therapy, medication dispensing takes place in various ways. Although ADEs can occur with each method, standardizing medication labels for vials and IV therapy throughout a single hospital or an entire health system can reduce their occurrence.
Medication Labels For Vials
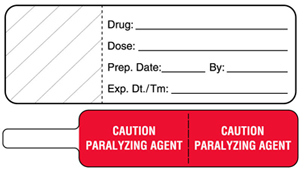 For example, vials from the pharmacy include medication labels containing key patient information, the drug name, dosage, route and more. Plus, colors designating a particular drug class help differentiate the medications. Although many organizations use ASTM standards, different color coding processes create potential confusions that can lead to medication errors.
For example, vials from the pharmacy include medication labels containing key patient information, the drug name, dosage, route and more. Plus, colors designating a particular drug class help differentiate the medications. Although many organizations use ASTM standards, different color coding processes create potential confusions that can lead to medication errors.
Labeling IV Tubing
In addition, labeling IV tubing allows nurses to better manage the flow of medication into the IV lines. This ensures:
- Dispensing The Same Drug - IV bags and lines get tangled. A label placed at the top of the line and/or closest to the insertion point helps ensure proper dispensing
- Same Dose - Medication dosage is often changed from shift-to-shift. Noting the dose on the line and bag safeguards consistent medication management
- Time managed - Start and end times are critical in ensuring the proper dosage of the medication is received
Implementing an effective standardized process starts with involving the right players. Scheduling a review with the nursing and pain management staff will ensure a positive outcome for all. In fact, simple words and phrases on labels can have multiple meanings. It’s essential to discuss those differences and establish common ground prior to implementing changes.
Change Minder Labels
Another component of IV management are regular changes to prevent infection. A Change Minder label reminds the medical staff that the IV needs to be changed on a specific time or date. But, without a consistent process, this seemingly easy way to communicate information can be a cause of misinterpretations. For example, do you use military time or regular time? Is the change date an actual day or a date? Each practice is appropriate but when the clinical staff engages with different departments or facilities that use alternative methods, it’s a recipe for medication errors.
In fact, nursing departments need line and IV label guidelines that identify the specific information needed and how to fill it.
Wrong Route Of Administration
 Administering a drug using the wrong route of administration is another common problem. Moreover, the FDA cited that it’s the cause of 16% of medication errors. This includes a number of issues such as:
Administering a drug using the wrong route of administration is another common problem. Moreover, the FDA cited that it’s the cause of 16% of medication errors. This includes a number of issues such as:
- Swallowing a tablet instead of letting it absorb under the tongue
- Ingesting a liquid intended for injection or as a nasal spray
In fact, clearly communicating on the container how to dispense a drug will reduce medication errors.
Food And Drug Interactions
 Similar to the wrong route of administration, mixing certain foods and medications can cause an ADE. For example, vitamin K can render an anticoagulant such as Coumadin ineffective. Pairing it with leafy green vegetables, broccoli or Brussels sprouts can cause problems.
Similar to the wrong route of administration, mixing certain foods and medications can cause an ADE. For example, vitamin K can render an anticoagulant such as Coumadin ineffective. Pairing it with leafy green vegetables, broccoli or Brussels sprouts can cause problems.
Although formularies detail this information in medical record documentation, some pharmacies take it one step further and mark drugs with medication instruction labels. They serve as another checkpoint and assist the clinical staff in proper medication dispensing. But, if this practice differs between system hospitals and discharge nurses it creates a potential problem. When healthcare workers expect to see medication instructions on the drug itself they are more likely to overlook the precautions even though they appear in the medical records. Because a patients’ caregiver may differ, it’s essential to communicate this critical information verbally and document it.
How Information Technology Impacts Medication Label Standardization
Information technology advances safe medication dispensing. Computerized medication order entry (CPOE), clinical decision support systems (CDSS), barcode medication administration (BMA) and electronic health records (EHR) provide essential information and safeguards that reduce patient errors. But, in many cases, the information these systems deliver is output on a medication label. Although the information may be the same, if the output mechanism is different, the potential for error increases.
Lack Of Standardization
“A lack of care standardization has its roots in earlier days, when clinical decision-makers were trained at different institutions with different schools of thought. They brought these variations into practice with them and treated patients the way they were taught,” Nancy Lakier, RN, BSN, MBA, CEO of Novia Strategies stated. More recently, clinician prerogative has been exchanged for best practices.
And another step that will reduce these variations and further improve patient care is standardizing key processes. Medication labels are just one of the many important components that can improve patient care and safety.
United Ad Label
United Ad Label has extensive experience with implementing effective medication label processes in hospital and ambulatory settings. Contact us to learn more.