Improving primary care access is all about getting supply and demand in equilibrium. That’s one reason hospitals employ floating and temporary nursing staff, because it helps them manage supply and demand shifts. For example, sending a nurse from their home unit to one that requires more staff than originally scheduled, helps manage the increased patient load and care demand. Similarly, when unexpected staffing shortages occur, hospitals may utilize temporary nurses to manage the deficit. Ultimately, using floating and temporary nursing staff reduces the need for additional RNs, decreases overtime hours and lowers costs. Further, it provides opportunities for caregivers, including the option to work in multiple specialty areas and treat different kinds of patients. But, as they say, “there ain’t no such thing as a free lunch,” and with those benefits come challenges that can disrupt the model. In fact, these 3 underlying patient safety challenges that floating and temporary nursing staff face can impact job satisfaction and the patient experience.
Floating And Temporary Nursing Trends
Healthcare organizations are employing floating and temporary nursing staff with increasing frequency. To illustrate, temporary or supplemental nurses account for approximately 30% of the nursing workforce in the United States. And although floating staffs were common before COVID, their use increased during the pandemic. More than 60 percent reported “floating” across these multiple contexts last year, nearly two times the rate pre-pandemic. So the challenges that come with these staffing alternatives are not one off, instead they impact a wide scope of hospitals, caregivers and patients.
3 Patient Safety Challenges Floating & Temporary Nurses Face
 For any of us that have changed jobs, the first few days (maybe even weeks) brings stress that goes beyond your specific job responsibilities. And for a floating or temporary nurse, regardless of their experience level, the unknowns often cause stress that can impact job satisfaction and the patient experience. These three areas are typically problematic.
For any of us that have changed jobs, the first few days (maybe even weeks) brings stress that goes beyond your specific job responsibilities. And for a floating or temporary nurse, regardless of their experience level, the unknowns often cause stress that can impact job satisfaction and the patient experience. These three areas are typically problematic.
1) Handoffs
When the transfer of care shifts from one healthcare provider to another they “handoff” patient-specific information and knowledge to ensure the continuity and safety of that patient’s care. But risk is built into each handoff, because when handoffs are done poorly, important information does not get passed properly from one provider to the next. This result in errors, care omissions, treatment delays, inefficiencies from repeated work and more. In fact, The Institute of Medicine reported that communication failures, during handoffs, account for most adverse outcomes in hospitals.
2) Protocols
Standardization helps remove variation in practice. In general, variation in practice can mean variation in outcomes. Conversely, standardization in practice can standardize outcomes. That’s where protocols come in. As the uniformity of essential clinical care functions increases, the potential for errors decreases. 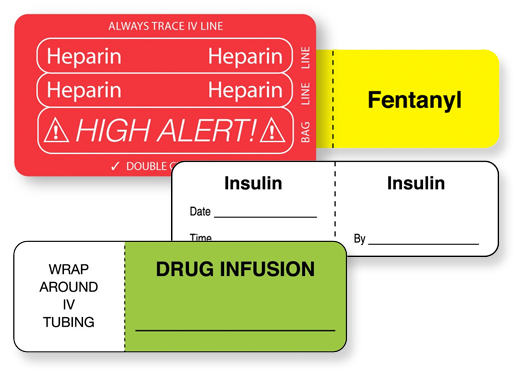 Yet, it’s not uncommon for certain protocols to differ from department to department. And even something that seems innocuous like an IV line label can create caregiver challenges when the colors, construction, formats and usage differ throughout the hospital. Consistent protocols make it more likely that patients will be cared for in the same manner regardless of where or by whom they are treated. Unfortunately, for floating nurses, inconsistencies lead to job dissatisfaction and errors.
Yet, it’s not uncommon for certain protocols to differ from department to department. And even something that seems innocuous like an IV line label can create caregiver challenges when the colors, construction, formats and usage differ throughout the hospital. Consistent protocols make it more likely that patients will be cared for in the same manner regardless of where or by whom they are treated. Unfortunately, for floating nurses, inconsistencies lead to job dissatisfaction and errors.
3) Orientation
From knowing the location of supplies to relationships with coworkers and supervisors, attempting to provide patient care in an unfamiliar environment can cause a number of issues. Negative perceptions about the assignment, lack of unit unfamiliarity and discomfort and stress experienced during the shift can manifest into bigger issues for patients and the providers. In fact, the seemingly simple task of retrieving supplies can turn unnecessarily complex and unproductive as nurses spend too much time searching for supplies and staff to assist them or answer questions. For example, in one study, inadequate orientation and training was the most common cause of sentinel events. Further, the lack of orientation negatively impacted nurse retention rates.
Steps To Improve Floating & Temporary Nurse Satisfaction & Patient Safety
Although handoffs during a shift change are a critical step that helps create a continuation of care, floating and temporary nurses need more. The best operations maximize job satisfaction and enhance patient safety that starts with standardizing processes when possible and implementing formal programs to address the challenges these nurses face.
Standardize Key Processes
Care delivery is a complex process and one that compounds in complexity when variables are introduced. And in addition to the complexities, modern healthcare is also high risk and error-prone.
Furthermore, ongoing changes in the healthcare landscape create a different set of challenges. For example, as health systems grow or merge, and the number of floating and temporary nurses that serve various facilities multiply, the potential to inject variables into care delivery increases.
But, standardizing key processes has proven to reduce these problems. In fact, Idaho based St. Luke’s Health System found that reducing care variations helped them reduce in-hospital deaths, reduce complications and shorten length of stay. You can read more about effective standardization steps here.
Develop A Structured Program
Unfortunately, many hospitals don’t have a structured process to onboard floating and temporary nurses into different units. But, for the healthcare organizations that do, nursing job satisfaction and retention rates increase as does patient satisfaction.
When developing an onboarding program, use these best practices:
- Standardize key processes
- Conduct a guided tour of the unit for first timers and nurses who haven’t had recent assignments in a unit.
- Develop unit specific checklists that include rounding schedules, the location of consent forms, the label colors on lab tubes and more. This study on creating a positive float experience details additional important points to cover.
- Review protocols. Although a basic overview is important, protocol overviews are even more essential when they aren’t consistent throughout the system. For example, if a patient requires an IV, reviewing line identification, how the date and time are identified, ASTM color choice and more are essential data points.
- Develop a network of mentors that know the unit and can support the floating or temporary nurse when they have questions.
These steps don’t guarantee that every floating nurse will prefer the experience vs. their home unit nor does it guarantee stellar patient satisfaction, but it does favorably impact both areas. Plus, the investments you make in a program like this pays dividends. The 2020 NSI National Health Care Retention & RN Staffing Report details that the average cost of turnover for a bedside RN is $44,400. In addition to the cost, in the current environment it’s especially critical to retain your staff.
United Ad Label
United Ad Label has extensive experience working with risk management and nurses on standardizing medication protocols and developing plans that meet the needs of caregivers and patients. Contact us to learn more.
